By: Karine Cohen-Solal, PhD
At the Thirteenth Annual Meeting of the Society of Hematologic Oncology (SOHO 2025), a new pilot program debuted to educate and empower the next generation of clinicians treating patients with relapsed or refractory (R/R) chronic lymphocytic leukemia/small lymphocytic leukemia (CLL/SLL).

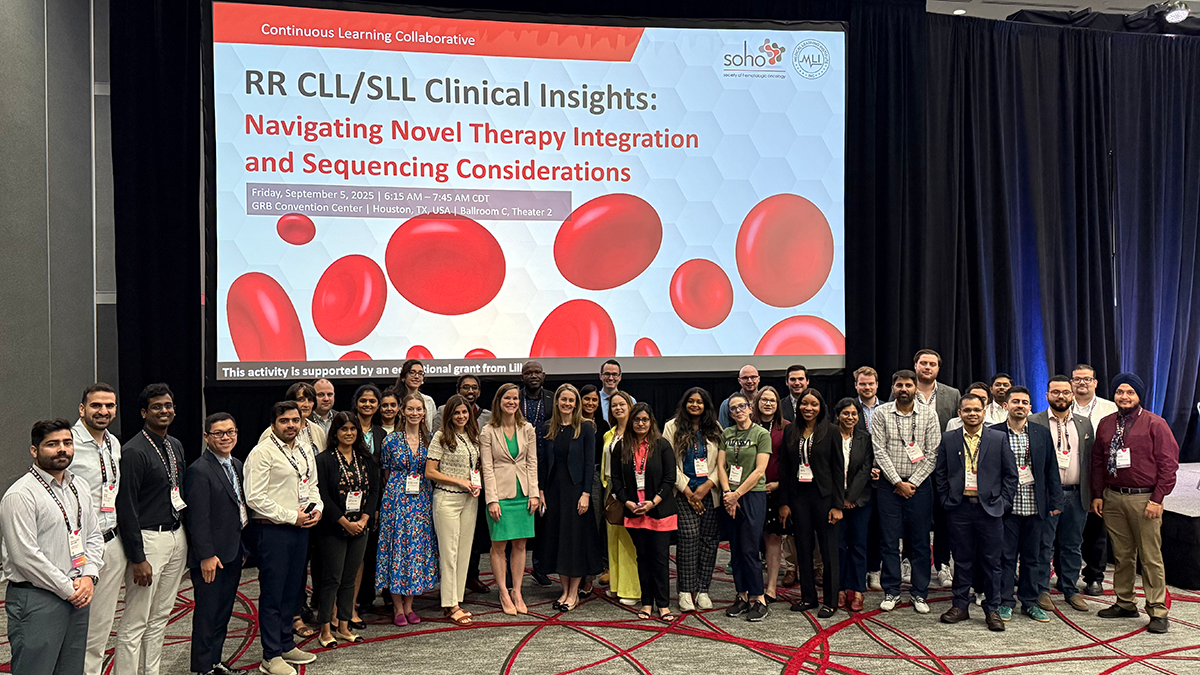
The Continuous Learning Collaborative (CLC), titled “R/R CLL/SLL Clinical Insights: Navigating Novel Therapy Integration and Sequencing Considerations,” is a partnership between SOHO and Medical Learning Institute (MLI) created for early-career clinicians (those within 10 years of practice) working in community or smaller academic settings.
In the first phase, insight was collected from the cohort of 25 participants during the summer of 2025. The second phase of the pilot study was intended to extend the reach of the program to clinicians with longer time in practice. That was achieved with a live intensive at SOHO 2025, which was open to all SOHO attendees, some of whom have been in practice for over 15 years.
Phase 1 insights
Launched in summer 2025, the initiative engaged 25 young investigators in phase 1 to collect real-world, practice-based insights that informed the design of the subsequent live intensive. Participants contributed de-identified electronic health records (EHR) from five of their own patients, responses to interactive case simulations via MLI’s Build Your Own Case Study™ (BYOCS™) platform; and detailed surveys capturing current R/R CLL/SLL treatment patterns and approaches.
Analysis of these inputs revealed the following important trends:
- Participants, though early in their careers, consistently ordered key prognostic tests, including del(17p), TP53, and IGHV tests. This aligns with guidelines favoring risk-adapted approaches.
- Acalabrutinib and venetoclax-based therapies dominated prescribing patterns (84% each), with pirtobrutinib at 48%, indicating uptake post-accelerated approval. International respondents highlighted access barriers in resource-limited settings, including Pakistan and Egypt.
- Participants reported atrial fibrillation (84%), bleeding (56%), and infections (56%) as being the most challenging BTKi-related Adverse event (AEs) /toxicities.
- Most participants noted integrating patient-specific factors into treatment decisions, including preference for oral administration, time-limited duration of regimens, refusal of infusion/IV, quality of life, and convenience.
- Data from 116 patient records revealed a progression from ibrutinib-dominant as first-line therapy to acalabrutinib/zanubrutinib/venetoclax in second and third lines, with pirtobrutinib emerging in later lines.
- Growing interest in clinical trials (24% of participants) and novel modality like lisocabtagene maraleucel (8%) prescribed/selected during the last six months indicate a forward-looking approach from participants in the adoption of CAR-T and other innovative treatments.
Participants also identified educational needs. One learner noted, “To optimize the use of BTKis, including newer agents like pirtobrutinib, the most helpful resources would include clear, clinical algorithms for treatment sequencing, especially in the context of prior BTKi exposure or resistance. Guidance on when and how to perform molecular resistance testing would be valuable, as would practical tools for managing common toxicities such as atrial fibrillation, hypertension, and bleeding.”
Phase 2: live intensive at SOHO 2025
The 90-minute live session integrated phase 1 insights, allowing participants to apply the latest evidence-based guidelines to real-world patient scenarios. Activities included case-based decision-making and immediate expert feedback. Group discussions addressed AE management and sequencing challenges.
Key findings are as follows:
- All attendees (100%) reported intent to enhance their practice via guideline adherence, evidence-based personalization, and patient-centered decision-making.
- All learners (100%) rated the activity highly for achieving the learning objectives, faculty expertise, engaging format, teaching and learning methods, and bias-free content. One participant commented, “It will impact not only my practice but first of all the life of the patients.”
- Comments included incorporating evidence on adverse events, shared decision-making, and differences between BTKi-refractory and BTKi-exposed disease to help improve patient outcomes.
- In the preceding six months, venetoclax-containing regimens (70%) and covalent BTKis such as acalabrutinib and ibrutinib (57% each) were most frequently prescribed, followed by zanubrutinib (38%). Noncovalent BTKis (eg, pirtobrutinib; 24%) were primarily used for efficacy, based on recent evidence (19%) or prior resistance to BTKis (46%).
- Similarly to the data from the 25 learner-cohort from phase 1, clinical trials (27% of participants)
and lisocabtagene maraleucel (8%) were selected or prescribed during the last six months, confirming a positive approach toward emerging treatment modalities and agents or regimens. - Atrial fibrillation (46%) and hypertension (30%) were the most challenging BTKi-related adverse events to manage. Bleeding, neutropenia, and arthralgias/myalgias (27% each) were also frequently cited.
- Learners preferred noncovalent or second-generation covalent BTKis for younger or intolerant patients, venetoclax-based regimens for moderately fit or travel-oriented patients, and zanubrutinib for elderly, frail, or relapse-concerned patients.
- Learners identified limited access to multidisciplinary care (25%), patient adherence (20%), and systemic issues such as insurance and reimbursement (20%) as major barriers. The program provided strategies to overcome these barriers for 70% of learners.
- Learner questions reflected ongoing uncertainty about post-resistance therapy sequencing, management of atrial fibrillation and CNS disease, retreatment indications, and global access disparities.
Group-based discussions during the live intensive
Each participant met one-on-one with a faculty member for 30 minutes, spending 15 minutes on adverse event management and 15 minutes on treatment sequencing. Discussions were related to the three cases in MLI’s BYOCS™ activity, along with participants’ clinical challenges.
Interests are listed as follows:
- Preference for acalabrutinib versus zanubrutinib based on cardiac toxicity profiles.
- Rationale for shifting from ibrutinib to second-generation covalent and noncovalent BTKis.
- Use of obinutuzumab with BTKis for cytoreduction in high disease burden.
- Necessity and criteria for PJP prophylaxis in patients treated with BTKis.
- Concerns regarding PLCG2 mutations and their impact on potential resistance to pirtobrutinib.
- Criteria for identifying patients suitable for allogeneic stem cell transplantation.
- Exploration of triplet combinations in R/R settings.
- Optimal timing for incorporating obinutuzumab into venetoclax-based regimens.
- Availability and role of BTK-resistance mutation testing in treatment decisions.
Conclusion
The pilot program showed that structured, multiphase learning can engage clinicians at all career stages and address real-world challenges in managing R/R CLL/SLL. Using EHR and survey data, case simulations, and expert feedback, the program reinforced evidence-based treatment sequencing, AE management, and patient-centered care. Early data suggest such initiatives can improve guideline adherence and patient outcomes across settings.
This article is the first of a series of three on the SOHO-MLI initiative, “R/R CLL/SLL Clinical Insights: Navigating Novel Therapy Integration and Sequencing Considerations.”
About the author
 Karine Cohen-Solal, PhD, is an experienced scientific and medical writer with extensive expertise in oncology, dedicated to advancing cancercare through clear, evidence-based communication and continuing medical education. Drawing on over 20 years of experience in oncology research, combines deep scientific insight with exceptional writing skills to translate complex discoveries into meaningful narratives that inform clinical practice changes and ultimately elevate patient outcomes.
Karine Cohen-Solal, PhD, is an experienced scientific and medical writer with extensive expertise in oncology, dedicated to advancing cancercare through clear, evidence-based communication and continuing medical education. Drawing on over 20 years of experience in oncology research, combines deep scientific insight with exceptional writing skills to translate complex discoveries into meaningful narratives that inform clinical practice changes and ultimately elevate patient outcomes.